
 Product Name: Hepatitis B Vaccine
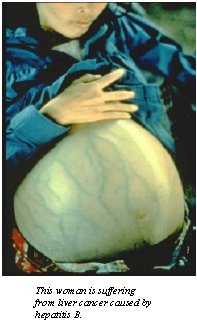
Product Name: Hepatitis B VaccineCommercial Name: Hepatavax B Date of Licensure: 1981 Company of Manufacture: Merck Sharp and Dohme Type of product: This first-generation vaccine was prepared from 22nM HBsAg particles purified from plasma donations from chronic HBV carriers. These preparations are safe and immunogenic, but have been replaced in most countries by recombinant vaccines produced by the expression of recombinant HBsAg in yeast cells. Target microorganism/associated disease: Hepatitis B virus (HBV) is transmitted by blood-to-blood and sexual contact and is an important cause of acute and chronic viral infection of the liver in many countries. The clinical features of acute hepatitis B infection resemble those caused by other viral hepatitis viruses. The HBV virus persists in approximately 5-10% of healthy adults, and in as many as 90% of infants infected at birth. Persistent carriage of hepatitis B, defined by the presence of hepatitis B surface antigen (HBsAg) in serum for more than 6 months, has been estimated to affect about 350 million people worldwide, although not all carriers can transmit the virus to others. Long-term continuing HBV replication can result in chronic liver disease, cirrhosis, and hepatocellular carcinoma, and results in 1-2 million deaths per year. Primary liver cancer is one of the 10 most common cancers worldwide, and currently 80% of such cancers are ascribed to persistent infection with HBV. Reason for development: Soldiers are at risk for exposure to HBV-contaminated blood and body fluids during battle (and sexual intercourse). Acute hepatitis was one of the main causes of illness among military members during the Vietnam war. A significant part of this was probably a consequence of contaminated needle use. Some service members from Vietnam and other wars continue injected drug use after returning to the U.S., and remained at risk from hepatitis B from shared needles. Role of Department of Defense in product development: Although development and testing of HBV vaccines have not involved military scientists, DoD contributed to epidemiology and HBV subtyping efforts. The U.S. military became focused on hepatitis B after the summer of 1942, when 50,000 cases of jaundice and 62 deaths occurred among soldiers vaccinated with the yellow fever vaccine. Investigators attributed the illness to a virus transmitted from human serum used in vaccine manufacture. The epidemic ceased after suspect vaccine lots were destroyed, and a human serum-free process was utilized. Investigations of stored samples many years later confirmed that the causative agent was HBV. Beginning in 1944 and continuing through the 1970's, the U.S. Army Surgeon General's office supported studies at Yale University and the Willowbrook State Hospital in New York which characterized the epidemiology and required immunoprophylaxis for different viral causes of epidemic hepatitis, including hepatitis B. Following Blumberg's discovery of the Australia antigen (HAA; now known as HBsAg) in 1965, the association of this antigen with hepatitis B was recognized, which made possible additional epidemiologic studies linking hepatitis B with intravenous drug abuse and sexual exposure. In the late 1960s, scientists at the U.S. Army Medical Research Laboratory at Fort Knox, Kentucky collaborated in a study of more than 1600 members of the Armored Brigade; the cohort included both soldiers who had recently returned from Vietnam, and recruits who had not yet been to southeast Asia. A significantly higher frequency of HBsAg carriers among the returnees (about 0.7%) than among the recruits (0.2%) was noted. In the early 1970s a second larger study involving nearly 20,000 Vietnam War returnees and recruits was initiated, which also incorporated data from returnees participating in a drug rehabilitation program. The higher HBsAg rate among newly returned service members was attributed to HBV acquired via injected drug use, but some returnees initially testing positive eventually became HBsAg negative due to presumed recovery from HBV. Current HBV vaccines utilize subtype "adw". Investigators at the Walter Reed Army Institute of Research carried out early work on subtyping strains of HBsAg from different geographic regions, and first described the w" and "r" antigenic determinants. |
| Influenza | Rubella Vaccine | Adenovirus | Meningococcal | Hepatitus B | Oral Typhoid | Japanese encephalitis | Hepatitis A |
